Delayed Care Could Have a Long-Term Impact on Patient Health
By May 2020, nearly 40% of Americans had delayed their healthcare. From preventive wellness visits and diagnostic testing to appointments for managing chronic conditions, patients have been putting off care due to challenges caused by the COVID-19 pandemic.Weekly Census Bureau Survey Provides Timely Info on Households During COVID-19 Pandemic, U.S. Census Bureau, 2020
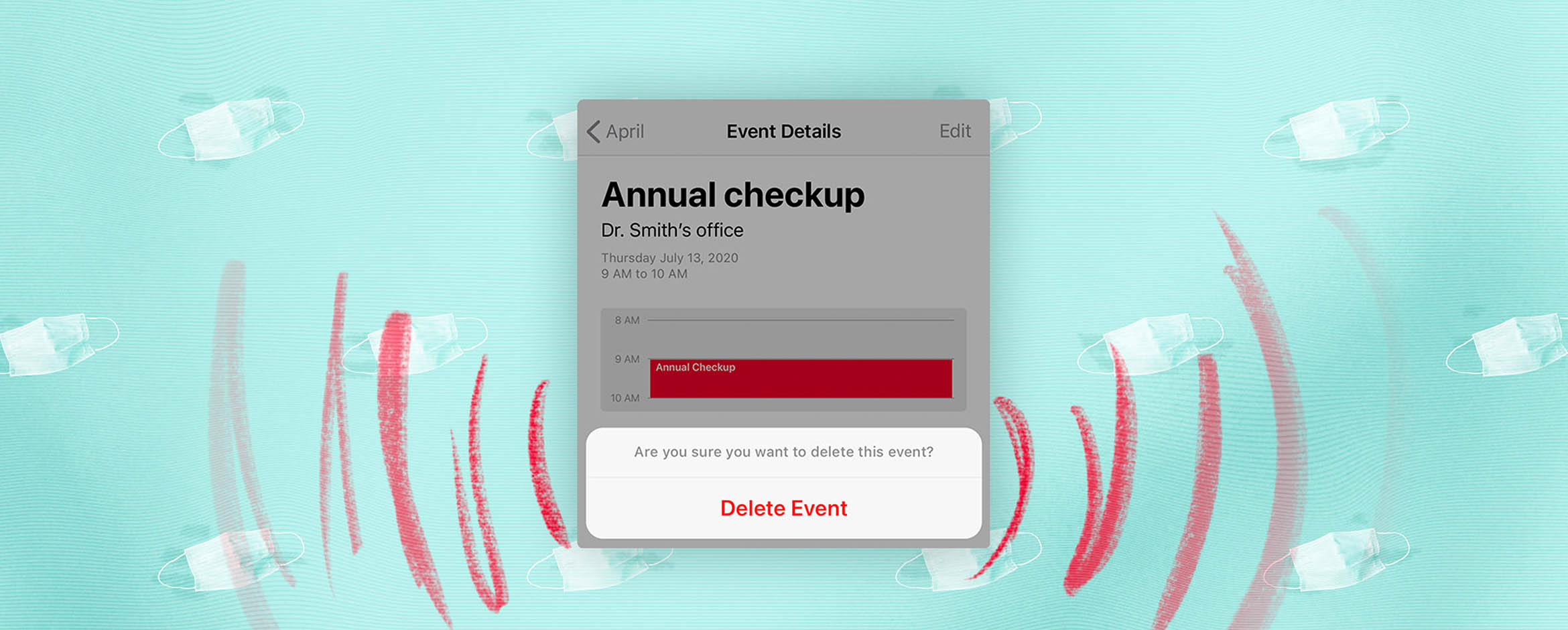
Many patients had no choice but to delay: As health systems prepared for a potential surge in COVID-19-related cases, and physicians’ offices closed temporarily throughout the country, we hit pause on non-emergent healthcare across the U.S.
In a survey conducted by CoverMyMeds in May of this year, 42% of respondents said they had to cancel or reschedule an in-person visit with their healthcare team due to COVID-19.CoverMyMeds COVID-19 Patient Survey
The dramatic decrease in patient visits this spring led to a financial crisis for health systems and providers. For the period of March through June, the American Hospital Association estimated $202.6 billion in losses for U.S. hospitals and health systems — an average of $50.7 billion per month.Hospitals and Health Systems Face Unprecedented Financial Pressures Due to COVID-19, American Hospital Association, 2020 Last month, they updated that estimate to include an additional minimum of $120.5 billion in losses from July to December 2020, or $20.1 billion per month.New AHA Report Finds Losses Deepen for Hospitals and Health Systems Due to COVID-19, American Hospital Association, 2020
Yet, while the financial impact on the industry has been massive, the long-term impact may be even more significant for patients. Delaying care now could result in serious health consequences in the future.
As Americans consider returning to their providers’ offices in the coming months, it’s the responsibility of all stakeholders in a patient’s journey to help diminish medication access barriers facing patients.
From transparency to affordability, healthcare IT solutions offer strategies to help patients in these unprecedented times. Innovation is likely to be a welcomed byproduct of COVID-19 — and will serve to benefit the overall patient experience.
Fear and affordability are factors in patients delaying care
Months after the first COVID-19 case appeared in the U.S., healthcare has started to find a new normal. Telehealth adoption is high, and new measures are in place to ensure patient and staff safety. As regular office visits have returned to operation, health systems across the U.S. have encouraged their patients to resume care. (McKesson, with 10 other healthcare organizations, recently launched the Stop Medical Distancing campaign.)
But many patients, concerned for their wellbeing amid a pandemic — or now un- or underinsured due to a COVID-19-related job loss 9.2 Million workers likely lost their employer-provided health insurance in the past four weeks, Economic Policy Institute, 2020 — are continuing to delay care. Some patients may even ignore potentially serious signs of illness, like the early symptoms of a heart attack or stroke.The Untold Toll — The Pandemic’s Effects on Patients without COVID-19, The New England Journal of Medicine, 2020
In May, Vanderbilt University Medical Center released the results of a survey of more than 1,300 patients. They discovered patients’ most common concern is a fear of contracting COVID-19 from another patient. As stay-at-home orders relaxed, 66% of survey respondents said they plan to resume “normal” care within a month, while 93% said they’d seek care for serious conditions within a month. When asked about elective screenings, however, that figure dropped to 37%.Patient survey reveals COVID-19 concerns and guides communication efforts, Vanderbilt University Medical Center, 2020
In our survey, 89% of respondents reported at least some financial impact from COVID-19, making access to care they can afford more difficult than before.CoverMyMeds COVID-19 Patient Survey, 2020 COVID-19 has also impacted patients’ access to their prescription medications: 34% of survey respondents said they’ve had trouble affording their medications — or have skipped picking up a prescription altogether due to its out-of-pocket cost.CoverMyMeds COVID-19 Patient Survey, 2020 27% reported they simply don’t feel safe making a trip to the pharmacy.CoverMyMeds COVID-19 Patient Survey, 2020
These trends may have far-reaching consequences for patients’ health. A Kaiser Family Foundation poll conducted in May found that 48% of Americans said that they or a family member delayed medical care due to COVID-19, with 11% reporting a condition worsening as a result of this delay.KFF Health Tracking Poll – May 2020
Of those survey respondents who reported cancelling or delaying in-person care, 55% identified themselves as cancer patients.CoverMyMeds COVID-19 Patient Survey, 2020
Norman Sharpless, director of the National Cancer Institute, said in an editorial this month that cancers undiagnosed now will come to light at a later stage and with worse prognoses. He predicts the number of deaths from breast and colorectal cancer in the U.S. will increase by nearly 10,000 over the next decade due to missed diagnoses.COVID-19 and cancer, Science magazine, 2020
*Having more information upfront can help a patient make the best decision for their current circumstance and support long term adherence to therapy. *
Telehealth is a critical part of the solution
Over the last few months, telehealth has been an essential alternative for providers and patients, with use of virtual visits increasing by at least 50% in March alone.Telehealth visits are booming as doctors and patients embrace distancing amid the coronavirus crisis, CNBC, 2020 Since the beginning of the pandemic, 44% of patients surveyed said their doctor had replaced in-person visits with telehealth services, while 42% responded that they had a telehealth appointment scheduled due to COVID-19.CoverMyMeds COVID-19 Patient Survey, 2020
While telehealth does allow much of the patient journey — from consultation to prescribing — to take place without the patient ever leaving home, a lack of crucial conversations that happen in a more connected setting could leave a patient with unanswered questions on medication cost and convenience.
Technology, including prescription decision support tools, can help provide seamless, transparent communication. Real-time benefit check (RTBC) technologies can facilitate a discussion between provider and patient about their prescription options.
With an integrated RTBC tool, providers can view and evaluate patient-specific benefit and cash price options for prescriptions, as well as pharmacy-specific information, like home delivery and mail-order options.
Having more information upfront can help a patient make the best decision for their current circumstance and support long term adherence to therapy. In a case study conducted by CoverMyMeds, patients whose providers used an RTBC solution reported a 19% increase in adherence compared to those who did not.Improving Prescription Decision Support with RxBenefit Clarity, CoverMyMeds, 2019
Solutions that prioritize patient choice enable shared decision making between the patient and provider including medication selection and method of payment, so that they can continue living healthy lives — pandemic or not.
What's next in healthcare?
We asked patients which COVID-19-related healthcare adaptations they’d like to see continue in the future. Here’s what they saidCoverMyMeds COVID-19 Patient Survey, 2020:
- 54%: Fewer in-person visits with my provider
- 40%: Fewer in-person visits to the pharmacy
- 63%: Longer prescription fills (90-days vs. 3-day fills)
Many retail pharmacies have launched prescription home delivery services, or waived fees for existing services to better serve patients staying at home. Of patients surveyed, 43% showed interest in permanently switching to a pharmacy home-delivery option for their prescription medications.CoverMyMeds COVID-19 Patient Survey, 2020
To afford medications during the pandemic, 77% of patients reported using a cash price program, copay card or manufacturer patient assistance program. Additionally, 84% said they’ll continue to seek out and use cost-saving methods moving forward.CoverMyMeds COVID-19 Patient Survey, 2020
The pandemic is likely to last at least another yearCOVID-19: The CIDRAP Viewpoint, Center for Infectious Disease Research and Policy, 2020, and patients can’t afford to continue to put their health on hold. More than ever before, patients need to be able to access — and afford — the care and medications they need.
Learn more about technology's impact on patient access.
The latest healthcare insights, floated right to your inbox.





